Understanding Genitourinary Syndrome of Menopause (GSM)
As a clinical nutritionist, I often encounter women experiencing various symptoms during p0erimenopause and menopause. One of the lesser-known but significant conditions is Genitourinary Syndrome of Menopause (GSM). GSM is a group of symptoms and clinical signs caused by the decline in estrogen and other sex steroids during menopause. Unlike other menopausal symptoms that may ease post-menopause, GSM tends to persist and even increase during the postmenopausal period.
What is GSM?
Previously referred to as vulvovaginal atrophy or atrophic vaginitis, GSM encompasses a range of symptoms that affect the genital and urinary systems due to estrogen deficiency. This condition can significantly impact a woman's quality of life, affecting daily activities, sexual health, and overall well-being.
Pathophysiology: What Happens to Your Body?
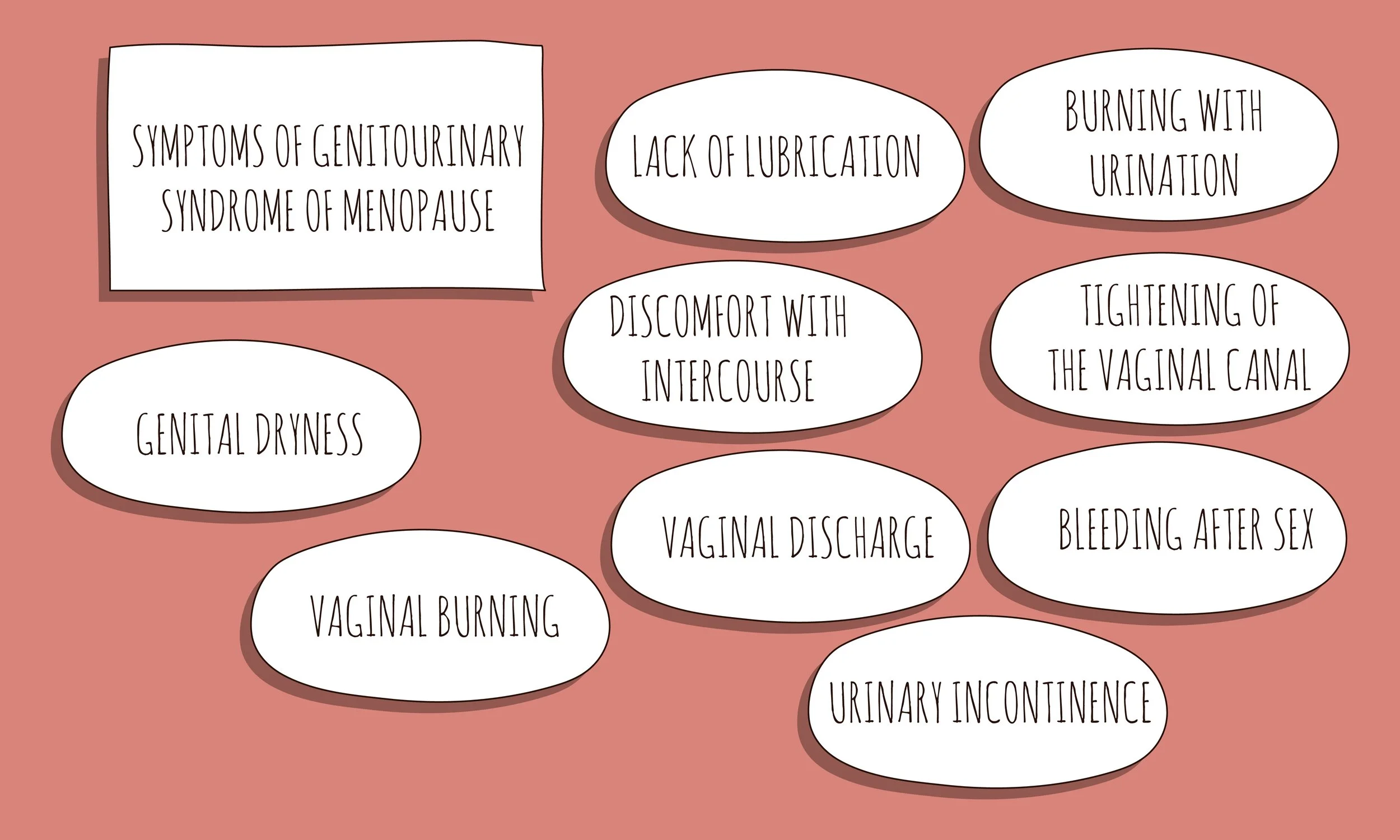
Estrogen is crucial for maintaining the health of the urogenital tract. It supports the vaginal wall's thickness, elasticity, and moisture, helps maintain an acidic vaginal pH, and enhances blood flow, which aids in lubrication. As estrogen levels decline, these supports diminish, leading to symptoms such as:
Vaginal dryness, burning, and irritation
Painful intercourse
Urinary frequency, urgency, and incontinence
Recurrent urinary tract infections
The Impact on Women's Health
In Australia, around 3.2 million women are experiencing symptoms of GSM. The Australian Institute of Health and Welfare estimates that over 50% of perimenopausal and postmenopausal women are affected. Despite the significant adverse effects on sexual health and daily activities, more than 60% of women with GSM do not discuss their symptoms with their GP. Shockingly, only 6%-7% of women experiencing GSM are receiving treatment.
Recognising and Diagnosing GSM
GSM is primarily diagnosed based on a detailed medical history and physical examination. Symptoms like vaginal dryness, burning, itching, and urinary issues should prompt further evaluation. During an exam, healthcare providers look for signs such as thinner, paler vaginal tissues and changes in vaginal pH.
Treatment Options: Finding Relief
Thankfully, there are various treatments available for GSM, ranging from over-the-counter options to prescription therapies:
Moisturisers and Lubricants: These provide relief from vaginal dryness and discomfort during intercourse. Regular use can significantly reduce symptoms.
Vitamins E and D: Topical application of Vitamin E and Vitamin D creams has shown potential benefits in lowering GSM symptoms by maintaining mucosal health and reducing inflammation.
Probiotics: These can help restore and maintain a healthy vaginal microbiome, potentially reducing GSM symptoms.
Vaginal Estrogen Therapy: Considered the gold standard, this therapy restores local estrogen levels, improving vaginal health and alleviating symptoms.
Dehydroepiandrosterone (DHEA): This hormone replacement therapy is an effective alternative for those who cannot use traditional estrogen-based treatments.
Take the Next Step: Book an Appointment
If you're experiencing any symptoms of GSM, it's essential to seek help. As a clinical nutritionist, I can provide guidance on managing these symptoms through diet, supplements and lifestyle changes. I can also provide information, guidance and referrals for other treatment options. Don't let GSM affect your quality of life—book an appointment today to discuss your symptoms and explore treatment options tailored to your needs.
Remember, you're not alone, and effective treatments are available to help you feel better. Let's work together to improve your health and well-being!